From The Washington State Wire
The Senate Behavioral Health Subcommittee held a meeting Monday morning to discuss the impact of the COVID-19 pandemic on behavioral health in Washington State. During the meeting, the committee heard from multiple panels on a range of topics including the state’s response, COVID’s impact on behavioral health clients and providers, and actions taken by Medicaid managed care plans.
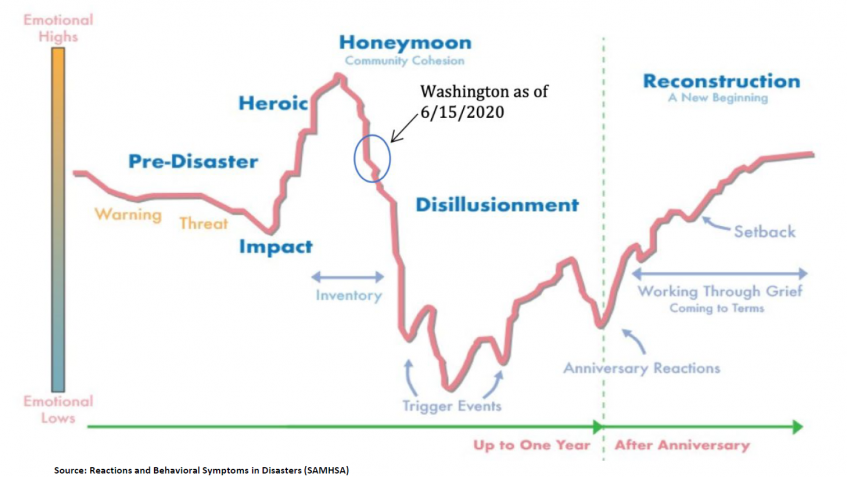
In a previously published version of the forecast (from May 15), DOH categorized Washington as being in the “honeymoon” phase, or the peak period of emotional highs during the pandemic. With the June 15 update, the state has dropped toward the disillusionment period and emotional lows are increasing. Covington says the disillusionment phase will be from about September to December for Washington.
“This is the period we’re really worried about as a state,” says Covington. “This is where we’ll likely see increased rates of depression, suicidal ideation, particularly increased substance use related to despair, and those sorts of topics. So, this is really a hard period for us as a state and one I want us to really be aware of.”

In her presentation on the impact of COVID-19, Kim Zacher, CEO of Comprehensive Life Resources, said her organization is seeing a behavioral health shift that follows along the path forecasted by DOH. She says in March and April, their clients were doing fairly well.
“They were rallying, they were experiencing the same sense of community and purpose that we all were. But really we’re starting to see an acceleration in those crisis calls, the decompensation, and I think just that extended experience of isolation, lack of face to face support…we really are seeing some impact,” says Zacher.
During her testimony, Zacher also discussed both the importance and limitations of telehealth. She says telehealth has been critical in helping people stay connected to services during the pandemic, but that it should be considered just one of the tools in the toolbox.
On one hand, telehealth can augment services and eliminate transportation struggles for some clients. On the other hand, says Zacher, many of the evidence-based practices being utilized haven’t been researched for delivery via telehealth. Also, trauma services or assessment of mental health symptoms can be difficult through telehealth, and Zacher says some clients are triggered by technology or may not engage due to anxiety or paranoia.
“For some people it’s a better means of connecting and for some people it makes it much more difficult,” she says.
The committee also heard an update on the actions taken by Medicaid MCOs during the pandemic to support members and providers. Bea Dixon, Behavioral Health Executive Director with UnitedHealthcare Community Plan of Washington, provided a summary of lessons learned during the pandemic:

Additional documents and presentations from the committee meeting are available here.
By Emily Boerger